About Root Canal
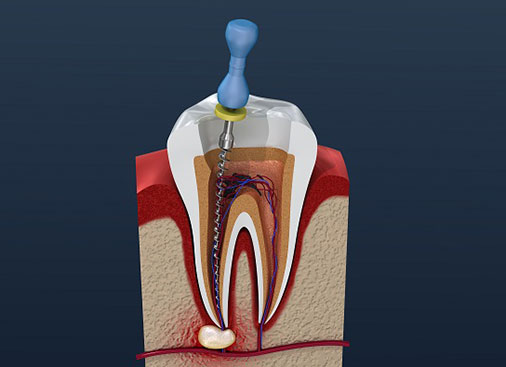
A root canal is a valuable dental procedure used to treat and preserve teeth with inflamed or infected roots. The pulp is the live tissue at the center of the tooth that contains nerves and blood vessels. When the pulp becomes inflamed or infected from a deep cavity or other reasons, patients can experience pain and swelling, and if left untreated can result in loss of the tooth. A root canal removes the damaged parts of the tooth as well as the inflamed or infected tissue from the center of the roots, taking you out of pain and getting rid of the infection. Root canal therapy must be followed up with a permanent filling or crown to seal the tooth and protect it from bacteria getting inside again.
Root Canal Retreatment
When a root canal treatment fails, the first course of action that is usually taken is root canal re-treatment. Root Canal Treatment can fail due to the following
- Canals were not cleaned and filled properly during first treatment.
- Small, curvy, and difficult to see canals could have been missed.
- New decay may have formed in the tooth infecting the root canal.
- A crack or fracture may have formed in the tooth.
- Permanent restoration was not completed in proper time after Root Canal Treatment.
The process is very similar to Root canal Treatment, the difference is that besides taking any remaining infected tissue out, the doctor has to take old filling material, any posts and crowns or any other obstacle in the pulp space out to be able to successfully disinfect and seal the area of the root canal.
After the root canal re-treatment is done your restorative dentist will place a crown to protect the tooth against fractures.
Apicoectomy
In the event that infection or a dental cyst persists in the jaw bone following root canal treatment, an apicoectomy may be indicated. It is a surgical procedure in which 3-4 mm of the root end is sectioned from the rest of the root. The existing root filling material is removed and the root end checked for any fractures under a high power microscope. Once cracks in the root are ruled out as the cause for the persistant infection, a bioceramic filling is placed to seal the end of the root from ingress of bacteria. Sometimes a bone graft and/or resorbable membrane is placed to aid in healing.
Trauma
When a tooth breaks or comes out of the mouth as a result of trauma, for example a baseball to the face, an elbow to the mouth in basketball, a car or bike accident, etc, it can be saved if proper treatment is provided in a timely manner. The International Association of Dental Traumatology (IADT) has a great website and a free app called “dental trauma first aid” that anyone can download to their phone. The website and app provide basic information to help you save the tooth of a loved one or friend if they ever experience dental trauma. As an endodontist, Drs Beatty and Wright have extensive knowledge in the treatment of teeth after dental trauma to give you correct information to best help retain your tooth/teeth. As members of the IADT, we are knowledgeable in the diagnosis, treatment and follow up protocols of 14 different types of dental trauma that may occur to both primary and permanent teeth.
Dental Resorption
Resorption refers to the loss of tooth (mostly root) structure as a result of a variety of influences. The most common types of resorption are:
- Inflammatory root resorption at the end of the root.
- External Cervical Invasive Resorption that begins at or below where the enamel of the tooth meets the root. Although we don’t know what causes this process to begin, it is more frequently associated with patients who have had internal bleaching to whiten teeth with a material called Superoxol. It is also more common in those persons who have had extensive orthodontics as an adult. The third associated is recent dental trauma. ECIR is classified into 4 stages of progression. Classes 1 and 2 are smaller and more successfully treated, but difficult to diagnose as this process has no symptoms. Classes 3 and 4 are frequently not treatable due to the extensive destruction of tooth structure that has already occurred.
- Internal Resorption looks like a growing balloon in the middle of the root canal. The dentinoclastic cells continue to remove root structure until either removed by calcium hydroxide paste during two stage root canal treatment, or are inactivated when the pulp tissue becomes necrotic (dies).
- Replacement Resorption occurs as a result of dental trauma. There are often no signs or symptoms. After irreversible damage to the periodontal ligament (PDL), the bone cells grow into spaces of the root. Untreated, this may result in the complete loss of the root and the visible tooth. (One reason why it is essential to see an endodontist after experiencing dental trauma for an evaluation)
Vital Pulp Therapy
When removal of part of the pulp tissue is required due to deep cavities in a young patient, it is sometimes possible to remove only the diseased part of the pulp and allow the rest of the root to develop to maturity. There is a specific protocol and use of bioceramic dental materials under specific conditions that are required to result in a predictable prognosis.
Laser Assisted Root Canal
The outcome of root canal treatment is based on efficient disinfection of the root canal system and prevention of reinfection .The laser irradiation has the potential to kill microorganisms and to remove debris and smear layer from the root canals.